JIA SOON LEN
Have you ever wondered what happens when our immune system turns its back and attacks our own body tissues and cells? Attacks on the normal body tissues and cells by our immune system lead to autoimmune disorders. The immune system can be divided broadly into two components: the innate and adaptive immune system. The innate immune system protects our body against a wide range of harmful microorganisms and elicits a fast response. In contrast, the adaptive immune system is slower but elicits specific and more effective responses. T cells, a component of the adaptive immune system, are involved in autoimmune diseases. Accumulating evidence points to dysregulated T cell metabolism in autoimmune disorders such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) patients. In the July issue of Cell Metabolism, Jenkins and colleagues investigated the effects of SGLT2 inhibitors on T cell function by assessing the levels of inflammatory molecules released, changes in proliferation, gene expression, and metabolism of T cells.
In the body, sodium-glucose co-transporter 2 (SGLT2) plays a major role in facilitating glucose reabsorption in the kidney. As the name implies, SGLT2 is involved in transporting glucose and sodium. In biology, the terms “luminal” and “basolateral” are frequently used to distinguish the sides of a membrane. The luminal membrane refers to the side of the cell membrane facing the lumen, the interior of a structure. The basolateral membrane refers to basal and lateral. The cell membrane’s basal side faces the direction opposite to the luminal (also called the apical) side. Transporters such as SGLT2 are necessary to transport sodium and glucose across the luminal membrane of a cell called the proximal convoluted tubule (PCT) cells, as the lipid-composed cell membrane is hydrophobic and impermeable to polar or charged molecules such as glucose and sodium (Na+), respectively. The movement of glucose into proximal convoluted tubule cells requires energy as it flows from low-concentration to high-concentration regions. This is like rolling a ball up a hill. Our body cleverly tackles this problem by coupling glucose transport with sodium, which moves from the high to the low-concentration region into the PCT cells. This is like coupling the rolling of a ball down a hill to drive the movement of another ball up the hill.
Type 2 diabetes is a disorder characterized by abnormally high blood glucose levels, which arise from the inability to respond to the insulin hormone. SGLT2 inhibitors such as canagliflozin and dapagliflozin are used to treat diabetes; these drugs prevent glucose reabsorption by the kidneys, allowing excess glucose to be removed from the body via urination, thereby lowering blood glucose in diabetic patients. There has been a recent attempt to repurpose other antidiabetic drugs, such as metformin, to treat autoimmune diseases, which was completely different from what metformin was originally designed for. The possibility of repurposing SGLT2 inhibitors (also antidiabetic drugs) for autoimmune diseases had not been well investigated before the study by Jenkins and coworkers.
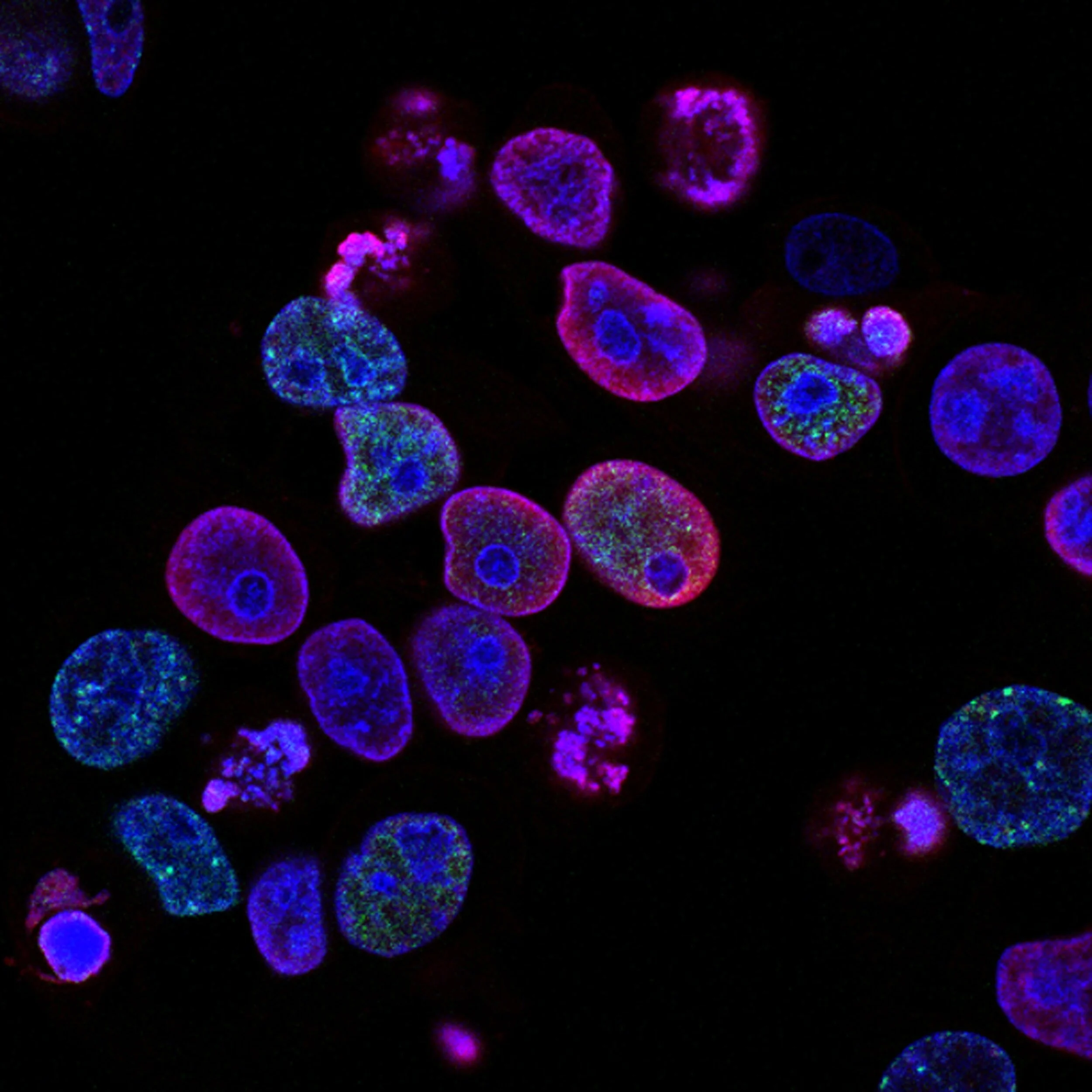
To test whether T cell activation is affected by SGLT2 inhibitors, Jenkins et al. incubated naïve CD4+ naïve T cells with known naïve CD4 T cell activators in the presence of either canagliflozin or dapagliflozin. T cells are white blood cells that develop in the thymus (an organ) to be functional in recognizing antigens while not attacking our body tissues or cells. Antigens are substances capable of eliciting an immune response, which can be derived from pathogens. The two well-known classes of T cells are CD4 and CD8 T cells. CD4 and CD8 refer to the coreceptor found on the surface of T cells. Every T cell has a T cell receptor (TCR) that allows it to recognize antigens presented by the major histocompatibility complex (MHC). MHCs are glycoproteins, and they are necessary to activate T cells because T cells only recognize antigens on MHC and not free antigens. This is similar to the fact that we can only consume food that is appropriately presented on plates and not floating freely in the air. CD4 and CD8 are called coreceptors because they bind to the same MHC as the TCR does and assist the TCR in recognizing peptides on either MHC class I or II, respectively. T cells either have CD4 or CD8 on their cell surface. These TCRs are like antennas that the cell uses to receive signals so that they can be instructed to perform certain functions when required. CD4 T cells are well-known for their helper functions as they activate other cells, for instance, to defend against infections by pathogens. CD8 T cell is renowned for its function in directly killing pathogen-infected cells. T cells that have yet to encounter TCR antigens after emerging from the thymus are called naïve. Subsequently, when these effector T cells encounter their corresponding antigens, they become activated and secrete effector molecules to carry out their functions.
Jenkins et al. observed reduced IL-2 levels and diminished expression of activation markers after naïve CD4 T cells were incubated with known activators in the presence of canagliflozin. IL-2 is known to be produced after naïve CD4 T cells become activated. As the name implies, T activation markers are indicators that T cells are in the activated state. This is similar to our facial impression in which we show our emotional state (e.g., anger). Taken together, these results suggest that T cell activation is impaired by canagliflozin. Jenkins and colleagues also observed the same effects of canagliflozin on CD8 T cells.
Interestingly, such effects were not seen when incubating naïve T cells with dapagliflozin (another SGLT2 inhibitor). Furthermore, the authors also noted canagliflozin downregulated the expression of genes involved in the cell cycle, and increased cell cycle inhibitor proteins, all of these results align with the observation that T cell proliferation is reduced. Cell cycle refers to the cycle in which cells grow in size and replicate their DNA and cellular organelles before undergoing cell division to give rise to two cells from a single cell. This cycle of cell growth and division is repeated during cell proliferation. Besides gene expression and protein level changes, the authors observed alterations to T cell metabolism after canagliflozin treatment. Some T cell metabolic changes reported in the study by Jenkins et al. include reduced adenosine triphosphate (ATP) production from glycolysis and alterations to the tricarboxylic acid cycle (TCA). ATP is the “energy currency” that cells use to power energy-requiring processes; ATP can be provided via glycolysis, a well-known process in which cells break down glucose. TCA is a series of chemical reactions in which cells generate ATP from fats, glucose, and proteins-derived metabolites.
In the same study, Jenkins et al. uncovered the mechanism underlying canagliflozin inhibition of T cell activation and effector functions. Appropriate TCR signaling is required for T cell activation and effector functions. The authors activated CD4 T cells with known T cell activators in the presence of canagliflozin and analyzed whether TCR signaling molecules were affected. The results indicate that canagliflozin inhibited the phosphorylation of TCR signaling molecules. Phosphorylation involves the addition of phosphate group(s) to the target. Phosphorylation of protein targets is known to cause conformational change in the protein and alter their functions or activities. As phosphorylation of TCR signaling molecules such as ZAP70 and LAT are necessary to propagate signals, these findings by Jenkins et al. suggest TCR signaling is inhibited by canagliflozin, thereby preventing subsequent T cell activation and effector functions.
Another critical finding by Jenkins and coworkers is that canagliflozin inhibited the activation of T cells isolated from systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) patients. Jenkins and colleagues incubated T cells from SLE and RA patients with known T cell activators in the presence with or without canagliflozin. Patient cells incubated in the presence of canagliflozin exhibited lower expression of T cell activation markers and decreased cytokines levels that T cells otherwise produce after activation. Cytokines are molecules that cells secrete to influence cellular behaviors. These cytokines, such as IL-17, are known to be pro-inflammatory and involved in autoimmune disorders such as RA.
Given canagliflozin’s capability to inhibit activation and effector functions of T cells obtained from SLE and RA patients, the findings by Jenkins et al. highlight canagliflozin’s potential to be repurposed to treat autoimmune disorders. However, as pointed out by the authors, the study did not investigate the effects of canagliflozin on cell types other than immune cells. Considering the complexity of autoimmune disorders such as SLE and RA, subsequent studies will conduct a more thorough evaluation of canagliflozin’s effects and whether they translate into better clinical outcomes for the patient Nevertheless, the work by Jenkins and colleagues opens up new possibilities for treating autoimmune disorders with drugs that authorities have approved and currently available. These drug repurposing efforts help advance the broadening of treatment options for autoimmune patients.
References:
Buang, N. et al. Type I interferons affect the metabolic fitness of CD8+ T cells from patients with systemic lupus erythematosus. Nature Communications 12, 1980 (2021).
Morel, L. Immunometabolism in systemic lupus erythematosus. Nature Reviews Rheumatology 13, 280–290 (2017).
Weyand, C. M., Zeisbrich, M. & Goronzy, J. J. Metabolic signatures of T-cells and macrophages in rheumatoid arthritis. Current Opinion in Immunology 46, 112–120 (2017).
Weyand, C. M. & Goronzy, J. J. Immunometabolism in early and late stages of rheumatoid arthritis. Nature Reviews Rheumatology 13, 291–301 (2017).
Jenkins, B. J. et al. Canagliflozin impairs T cell effector function via metabolic suppression in autoimmunity. Cell Metabolism 35, 1132-1146.e9 (2023).
Chao, E. C. & Henry, R. R. SGLT2 inhibition — a novel strategy for diabetes treatment. Nature Reviews Drug Discovery 9, 551–559 (2010).
Ferrannini, E. Sodium-Glucose Co-transporters and Their Inhibition: Clinical Physiology. Cell Metabolism 26, 27–38 (2017).
Sun, F. et al. Safety and efficacy of metformin in systemic lupus erythematosus: a multicentre, randomised, double-blind, placebo-controlled trial. The Lancet Rheumatology 2, e210–e216 (2020).
Foretz, M., Guigas, B. & Viollet, B. Metformin: update on mechanisms of action and repurposing potential. Nature Reviews Endocrinology (2023) doi:10.1038/s41574-023-00833-4.
Taams, L. S. Interleukin-17 in rheumatoid arthritis: Trials and tribulations. Journal of Experimental Medicine 217, e20192048 (2020).
Kaul, A. et al. Systemic lupus erythematosus. Nature Reviews Disease Primers 2, 16039 (2016).
Smolen, J. S. et al. Rheumatoid arthritis. Nature Reviews Disease Primers 4, 18001 (2018).