Syed Haider
Starfish can regrow limbs, some arthropods can regrow appendages, and certain worms can regenerate after being cut in half. Since humans share thousands of genes with these animals, it seems reasonable to look for evolutionary conservation in regeneration. Studying organ regeneration in animals to find solutions for humans is an important potential avenue for improving health and quality of life through better medical care, which has become a central quest in modern medicine as longevity has increased.
According to James Godwin, a researcher studying limb regeneration in salamanders at the Australian Regenerative Medicine Institute, regenerative methods observed in salamanders can be applied to human cells to accelerate wound healing. Studying the formation of scar tissue and regeneration in salamanders can help humans better understand chronic conditions – such as heart disease – and can inspire innovative therapies to enhance human life.
Also known as axolotls, Mexican salamanders (Ambystoma mexicanum) show remarkable regrowth of severed limbs. Axolotl hearts also exhibit the ability to regenerate at any life stage in the wake of tissue injury, says Godwin. His research revealed that a uniquely fast immune system lies at the core of regeneration in Mexican salamanders. He hopes to use axolotl physiology to illuminate dormant genetic pathways in humans that can accelerate the healing process.
Godwin’s team attributes axolotls’ regenerative abilities to an abundance of functional macrophages, which are immune cells that accumulate in mammalian tissue whenever an injury occurs. These cells usually arrive at an injured cell within two to four days and play an essential role in proper healing: activating adaptive immune responses. When bodily supplies of macrophages are depleted, axolotl limbs fail to grow back, whereas replenishing macrophages caused limbs to sprout more quickly again, indicating that macrophages are essential for regeneration. In the absence of macrophages, scars form at the site of injury; scars are thought to be the biggest hurdle for regenerating lost tissue in both axolotl and human organs.
Removal of scar tissue – lessons for humans?
The formation of scar tissue in the wake of damage to heart muscles is one of the major causes of heart disease in humans. Developing new organs or new heart muscle has been impossible in humans up until now, but studying regeneration of axolotl hearts shows a potential avenue for treatment of damaged human hearts. Heart disease is one of the leading causes of death worldwide; therefore, once pathways to eliminate scar tissue are better understood, treatment through regenerative techniques can be used to solve complications arising from scar tissue in human hearts
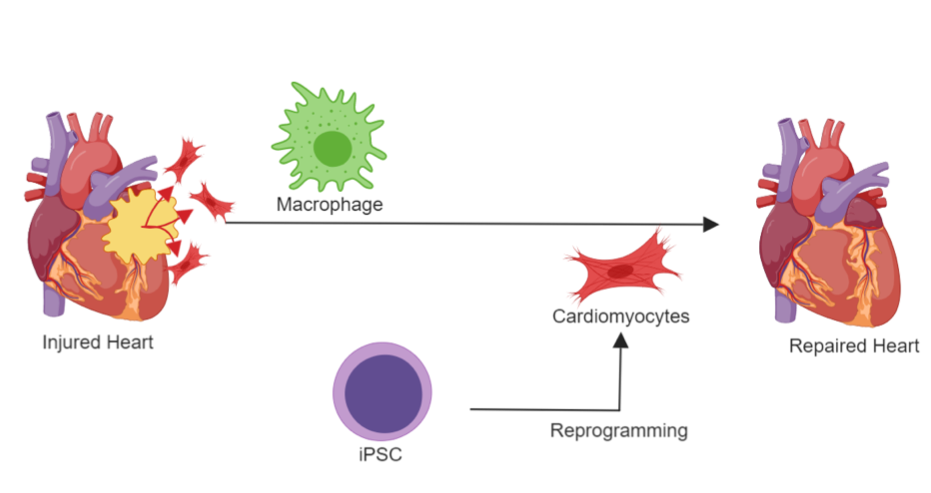
Heart muscle cells, also known as cardiomyocytes, die in the event of a heart attack in humans. Losing cardiomyocytes places an increasing burden on the remaining cells to pump blood according to Yueqiu Chen and his team, who studied the reprogramming of other cells to create new cardiomyocytes. Scar tissue forms in place of depleted cardiomyocytes, contributing to heart failure. Godwin says that in order to regenerate heart muscle, this scar tissue must be cleared first to improve blood flow in the circulatory system.
One method to manage scar tissue involves introduction of externally induced human pluripotent stem cells, according to a news report in Nature. These cells – generated from adult human cells and able to transform into multiple different cell types – provide a potential source of cardiomyocytes. Another method to manage scar tissue is through reprogramming cardiac fibroblasts (specialized cells that ensure normal working of the heart) to cardiomyocytes through providing the latter with external genes that determine the cells’ fate, according to Chen’s research.
Despite concerns, Japan has become the first country to legalize a procedure that is dependent on the above-mentioned technique of reprogramming cells into cardiomyocytes to regenerate heart muscles. As reported in Nature, these cells would be grafted into the heart in the form of thin sheets, each consisting of 100 million cells, and are expected to regenerate the damaged muscle without the need to introduce foreign materials.
So far, the application of regenerative techniques has shown positive results in animals such as axolotls and mice, but Chen’s group acknowledges that clinical trials on humans are needed before such techniques can be made widely available. But as research continues, cellular regeneration is moving to become a probable reality rather than a mere futuristic idea. Reprogramming heart cells could ultimately be a means of providing longer lives for people with heart conditions.