Author: Holly D. Thomas
Institution: St. Ambrose University
ABSTRACT
Amputees in underdeveloped areas often do not receive suitable prosthetic devices within the time frame needed for probable success. Typically, prostheses are either not secure or too constrictive of the residual limb. As a result, the constant friction and moisture collectionincrease the likelihood of skin breakdown. Furthermore, patients living in hot, humid climates are more prone to skin problemsdue to moisture and lack of proper hygiene. The objective of this project was to create an affordable and modular upper limb prosthetic socket for use by amputees in underdeveloped areas, specifically Brazil. The research group investigated common concerns with current products and materials used in such designs, gathered information about the country of interest, and used this information to develop quantifiable specifications for new socket designs. After a series of concept brainstorming and scoring, the team developed two socket concepts: (1) funnel-shaped holes and air pump system, and (2) open-frame design with breathable material and VELCRO® straps. Multiple three-dimensional models and prototypes consisting of wooden sockets with a TENCEL® interface for each of the two concepts allowed the team to diagnose potential obstacles. Further research and alterations may provide amputees in other underdeveloped areas with appropriate sockets for their climates and abilities.
INTRODUCTION
A large majority of the more than 40,000 individuals in the United States with major-limb loss will be implemented with a prosthetic device (Ziegler-Graham, MacKenzie, Ephraim, Travison, & Brookmeyer, 2008). In general, an upper limb prosthetic consists of a socket, a wrist unit, a forearm section or extension, a suspension system to secure the prosthesis, and a terminal device or hand (Strait, 2006). The socket component of the prosthetic is the main focus of this research. The socket is the interface that goes directly over the patient’s stump and connects to the terminal device at the opposing end (Strait, 2006).
The purpose of this project was to design an affordable, adjustable upper limb prosthetic socket for patients in underdeveloped areas. The socket must be able to withstand the hot, humid climate of the country and minimize the chance of skin breakdown caused by rubbing and moisture collection in the socket. Additionally, patients in Brazil have low access to hospitals and clinics, making frequent modifications and fittings nearly impossible. Therefore, the socket must maintain high functionality and comfort while reducing the need for constant adjustments.
BACKGROUND
According to Alley, Williams, Albuquerque, and Altobelli (2011), a traditional socket is made by first wrapping the residual limb in plaster wrap to define its shape, which generally has a circular cross section throughout. The plaster wrap shell is then filled with plaster that is slightly modified to accommodate bony prominences (Alley et al., 2011).This creates a model of the residual limb. The actual socket is created over the model using laminating or thermoforming plastic (Alley et al., 2011). In addition to this casting process, socket molds can also be made using computer-aided design, or CAD, which uses digital images of the residual limb to make the mold (Virginia Prosthetics, 2014). These traditional sockets apply concentrated loads near the end of the residual limb, rather than distributing the load uniformly throughout the entire limb. These concentrated loads can cause the amputee to experience discomfort and fatigue. For many patients, the initial effort needed to move their prosthetic is wasted in lost motion. According to Alley et al. (2011), “this lost motion occurs because the end of the humerus must compress the muscle and fat between the bone and the socket wall before force can be transmitted.” Reducing lost motion would help prevent fatigue and improve comfort while still meeting the objectives of a traditional socket.
According to Daly (2000), “the objectives of the socket in upper limb prosthetics are to support the terminal device in a functional position and to provide for range of motion (ROM) and grasp capability.” A suspension system must be used to securely hold the socket onto the residual limb. There are currently several different types of suspension systems in use. In developed countries, prosthetics are generally suspended either by a pin-locking mechanism or an airtight suction method, both of which require the use of a liner. A liner is similar to a sock placed over the patient’s skin underneath the socket. However, liners require daily cleaning order to minimize the risk of infection. In underdeveloped areas, the use of a liner is impractical due to hot, humid climates and a lack of proper hygiene. Therefore, suspension through figure-eight harnesses is more beneficial (American Prosthetics & Orthotics, personal communication, February 5, 2014). These types of harnesses are used to suspend body-powered prosthetics. In bodypowered prosthetics, all movement and manipulation of the prosthetic is done through movement of the opposing shoulder. They are less expensive than passive and electric prosthetics, and thus
more prominently used in developing areas.
In developing countries, the cost of a prosthetic can range from $125 to $1,875 USD (Strait, 2006). Even the cheapest prosthetic can be difficult to acquire and maintain, considering that the average annual family salary is only $300 USD in many povertystricken areas (Strait, 2006). Even if an individual has enough money to purchase a prosthetic, the probability of that individual actually obtaining a prosthetic and successfully using it is slim. Research has shown that prosthetics do not reach the majority of amputees in developing countries until after a year following their amputation (Strait, 2006). By this time, many patients have already learned to compensate for their lost limb, making it highly probable that they will reject the prosthetic. Because their survival requires quick adaptation to the situation, amputees are unlikely to have success with a prosthetic if more than six months have passed following the amputation (Strait, 2006).
According to a study by Østlie et al. (2012), roughly 13.4% of amputees will end up abandoning their prosthetic because discomfort and fatigue often outweigh the benefits that it offers. Østlie et al. (2012) also state that “the main reasons for secondary prosthesis rejection stated by the unilateral amputees were dissatisfaction with prosthetic comfort, function or control.” Even the individuals who continued to use their prosthetic device may not have considered their prosthetics to be free of flaws, although no studies have elaborated on long-term satisfaction of prosthetic use. Common priorities among prosthetic consumers include the weight of the device, the harness’s configuration and design, and temperature and moisture control (Biddiss, Beaton & Chau, 2007). Many users of body-powered prosthetics find that the weight of the prosthetic causes exhaustion and pain, a problem attributed mostly to the harness system. The lack of soft materials and harness options causes some patients to forgo using the prosthetic altogether (Biddiss et al., 2007).
According to Visscher et al. (2011), some form of skin irritation or breakdown due to prosthetic limbs can occur in up to 74% of patients. One of the main causes of these skin problems is a lack of proper hygiene, especially in underdeveloped countries. Blisters, cysts, and ulcers are caused by excessive shear stress and pressure on the skin (Sanders, Greve, Mitchell, & Zachariah, 1998). The properties of a material, including the static coefficient of friction, compressive stiffness, non-recovered strain, and moisture vapor transmission rate, greatly impact the shear distribution and pressure on an individual’s skin. These properties must be carefully considered when choosing an interface material in order to minimize the risk of tissue breakdown.
Static coefficient of friction (COF) is “the ratio of shear force to normal force necessary to initiate movement of the material relative to the skin,” as defined by Sanders et al., 1998. There are both advantages and disadvantages to having a low static COF. It is very effective at minimizing the risk of skin breakdown, but also results in a greater likelihood of skin slip, a condition that puts the underlying tissues at risk. A high COF reduces the chances of slipping, but to the extent where rubbing causes blisters and ulcers of the skin (Sanders et al., 1998). Therefore, it would be ideal to provide a common balance by using a material with an intermediate COF.
Sanders et al. (1998) define compressive stiffness as the “instantaneous slope of the stress-strain curve under compression loading.” To provide the amputee with a higher level of comfort than is found in current prosthetics, a material with a low compressive stiffness is necessary. This will provide a “cushioning effect on soft tissues” of the residual limb, and thus a higher level of comfort to the user (Sanders et al., 1998). Similarly, limiting the amount of non-recovered strain is essential for maintaining the original volume of the prosthetic. Non-recovered strain is a permanent decrease in the material’s thickness when subjected to a force (Sanders et al., 1998). In underprivileged areas where amputees do not have access to medical professionals capable of frequent refitting, the ability of the prosthetic to resist changes in volume is critical.
A final characteristic that is essential for an ideal interface is a high moisture vapor transmission rate (MVTR). MVTR is the rate at which water vapor passes through a substance (Protective Packaging Corporation, 2014). In this application, a high MVTR will allow perspiration and oils to dissipate through the interface material, keeping the residual limb dry and cool. If a material with a low MVTR is used, especially in a hot, humid climate, the perspiration will continue to settle on the skin of the residual limb, causing dangerous breakdown of the skin (Michaels, 2011). The research group created a table in Microsoft Excel to compare the properties of multiple material choices for the socket interface. The following materials were evaluated to determine whether they meet the ideal properties for this socket: (1) a medium COF, (2) a low compressive stiffness, (3) limited non-recovered strain, and (4) a high MVTR. If a material has the desired property, an “X” was placed in the appropriate cell. The complete table is shown in Table 1.
The comparison showed that spenco, poron, and silicone all possess the first three ideal properties. However, none of the materials evaluated have a high MVTR, which is crucial to minimize tissue breakdown. Therefore, a new material not listed in the table was necessary to meet all of the criteria.
MATERIALS AND METHODS
Evaluation of the Customer and Requirements
The direct customers for this research are upper limb amputees in Brazil and other developing areas. Secondary customers include the caretakers of the amputees, the hospital and clinic staff responsible for prosthetic adjustments and assisting the amputees, the prosthetists responsible for fitting the prosthetics, and the manufacturers of the prosthetics. For this prosthetic socket, the requirements include:
1. Affordable in underprivileged areas.
2. Modular to limit the number of necessary socket adjustments.
3. Breathable to limit the rubbing and moisture collection in th socket that causes skin breakdown.
4. Must enhance the patient’s level of independence and functionality compared to without a prosthetic device.
5. Easy to use and adjust.
6. Light and comfortable for the patient to wear for long periods of time.
7. Safe for both primary and secondary users. These criteria ensure that the benefits of the prosthetic to the amputee exceed any discomfort that he or she may feel. This will encourage the patient to not abandon the prosthetic.
Table 1. Ideal properties of possible socket interface materials. Spenco, poron, and silicone all have medium coefficients of friction, low compressive stiffness, and limited non-recovered strain. These characteristics are all properties necessary for the purpose of this socket. However, none of the materials have a high moisture vapor transmission rate, which is essential to minimizing skin breakdown. Therefore, a new material must be considered for this socket interface.
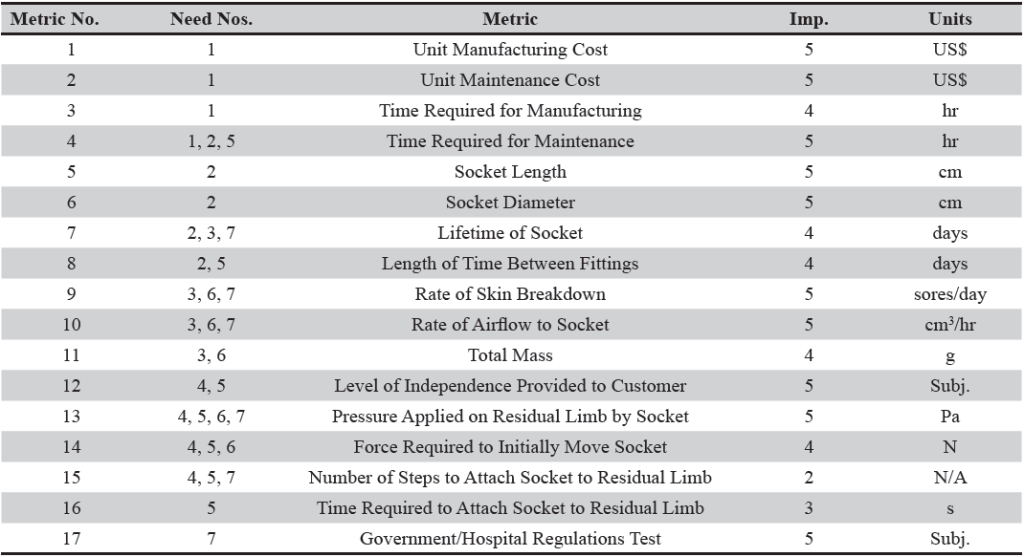
List of Metrics and Needs-Metrics Matrix
In order to quantify these requirements, a list of metrics was prepared. Seventeen metrics were defined based on the seven requirements of the socket. Each metric was given the proper units and classified by the needs it met. All 17 metrics were individually ranked by importance on a scale of one to five, with five being the most important. The prepared list of metrics is displayed in Table 2. This list was also used to create a needs metrics matrix for the socket. The needs-metrics matrix visually displays the needs that are met by each metric, shown in Table 3. The matrix also includes two benchmark products, the Patent Number 5,888,235 Body- Powered Prosthetic Arm (Sarcos, Inc., Salt Lake City, Utah) and the DynamicArm Above-Elbow Prosthesis (Ottobock©, USA). The ability of both products to meet each need is displayed in the matrix next to the metrics.
Table 2. List of metrics to quantify the socket requirements. These metrics were developed to assist in quantifying the seven socket requirements. The level of importance of each metric was ranked on a scale of one to five, with five being the most important. The units for each metric and the socket requirement number(s) are also presented.
Concept Brainstorming
After the required specifications for the socket were determined, multiple methods of concept brainstorming were used to generate ideas for developing a new prosthetic socket. A process known as brain-writing was used in the St. Ambrose University Design Lab classroom. During the brain-writing session, two of the most vital requirements for the socket were written on pieces of notebook paper. The two requirements believed to be most important and that could most benefit from this process were (1) the socket must provide good airflow in a hot, humid climate, and (2) the socket must be modular enough to not require frequent adjustments or fittings. The two pieces of paper were separately passed around the room to the Design Lab students. For approximately 20sec to 30sec, each student had the opportunity to write down any ideas he or she had for meeting these requirements. This process allowed for a larger population to contribute ideas for the product without fear of rejection. Some of the most beneficial ideas that stemmed from this session include:
• Cooling tubes running the length of the device to assist with airflow and minimizing perspiration in the socket.
• A built-in fan to assist with airflow in the socket.
• VELCRO® to allow for easy adjustment.
• Cotton, mesh, or pre-wrap material to keep the socket interface modular.
The ideas from the brain-writing session were further considered in another brainstorming session. Multiple ideas were combined to create new ideas that proved to be the most viable and successful. From this brainstorming session, four concepts for creating a breathable socket and four concepts for creating a modular socket were developed.
Concept Scoring
The four breathable socket concepts and four modular socket concepts were weighted and scored using concept scoring tables. The concepts were compared to a reference product, which is the currently available body-powered socket. The scale used to rate the concepts according to the selection criteria was a one to four scale, where one indicates that the concept inadequately meets the criterion, and four indicates that the concept exceedingly meets the criterion. For the breathable socket concepts, the highest total weighted scores were for the funnel-shaped holes design and the open-frame design with a breathable material. The modular socket concepts with the highest total weighted scores were the VELCRO ® straps and air pump. It was decided that these four concepts would be combined into new ideas and developed further, while modifications of the lower-ranking concepts would be terminated. In order to further develop the concepts to make a socket that is both breathable and modular, the highest-scoring concepts from each table were combined into two new concepts. These concepts were (1) funnel-shaped holes and air pump system, and (2) an open-frame VELCRO® design with a breathable material.
In the first design, the socket had funnel-shaped holes and an air pump system similar to the system currently used in walking boots. The funnel-shaped holes allowed airflow through the socket to the skin, while the air pump allowed the amputees to adjust the fit of the socket themselves. The open-frame VELCRO® design was based off of a back brace. There were horizontal structures at the top and bottom of the limb that were adjustable using VELCRO®, and these were connected by three or four vertical structures with metal stays. The breathable material covered the residual limb in a similar manner to the current socket interfaces. The open-frame design limited the amount of restrictive material covering the limb and allowed maximum airflow to prevent skin breakdown. The VELCRO® allowed the patient to adjust the socket themselves, and the breathable material further increased airflow to the limb. To compare these two ideas to each other and with the reference body-powered socket, a new concept scoring table was created.
The rankings of the two concept ideas were very close, so the decision was made to develop both designs into prototypes for better comparison of the viability and successfulness of the product concepts.
Materials Selection
A meeting was held with a prosthetist from American Prosthetics and Orthotics (2014) to determine the proper materials needed to ensure that the socket has the ability to attach to an end effector. After updating the prosthetist on the work accomplished thus far, it was confirmed that using a popular wood from Brazil called piacava to create the frame of the socket would be an effective and affordable option. However, piacava is not readily available in the United States, so a different wood with similar properties to piacava would be used in the initial sockets. Some lightweight, thin wooden rods and ductile twine were purchased to create a socket frame that could easily be made from piacava in Brazil.
Table 3. The needs-metrics matrix. This chart visually shows the needs that are met by each metric. Two benchmark products are also broken down in the chart using a one to five dot system, where five dots signifies that the product meets the need to the highest standard (Ottobock©, 2013; Jacobsen & Knutti, 1999).
From the discussion with American Prosthetics and Orthotics (2014), it was strongly recommended that the previous idea of silicone not be used in the socket for the following reasons: (1) silicone is generally only used to generate suspension through a liner rather than a harness system, and (2) using a layer of silicone on the outside of polytetrafluoroethylene, or PTFE, will cancel out the wicking properties of the PTFE by preventing the diffused moisture from evaporating into the environment.
Additionally, PTFE is generally fairly uncomfortable on the skin, so it was suggested that a more comfortable material that contains similar wicking properties be used. Through further material research, a man-made, environmentally-friendly material known as TENCEL® (Lenzing Group, Austria) was discovered. TENCEL® is made from the wood pulp of eucalyptus trees, which are highly prevalent in Brazil. Several studies have shown that TENCEL® has a smoother surface than cotton and wool, as well as far superior moisture management properties (Männer, Schuster, Suchomel, Gürtler, & Firgo, 2004). According to Männer et al. (2004), “within 20 seconds the lyocell [another name for TENCEL®] fabric reaches a maximum absorption capacity of 380% moisture, which is absorbed in a homogenous distribution over the entire surface. Cotton and polyester show a moisture uptake of only 16 to 19%.”
A study by Kandhavadivu (2013) on the optimal blend of TENCEL® and polyester to revealed that a “higher proportion of polyester leads to poor comfort characteristics of the fabric, which is not suitable for hospital textiles. Hence polyester blend ratio is restricted to 15% and 30%.” Brazil’s favorable environment allows for vast plantations of eucalyptus trees, making TENCEL® a highly accessible and affordable material. COOLMAX® (INVISTA, USA) was chosen as the socket interface for this project because it has similar properties to TENCEL®, and it is already available in an upper-limb prosthetic sock that does not require any alterations. TENCEL® socks would have needed to be altered, and thus were impractical for the purpose of this project.
In order to learn how the air pump mechanism works, a medical walking boot was reverse engineered. The purpose for reverse engineering the walking boot was to determine if the air pump system in the boot could be incorporated into the socket, or if a new one had to be created. The air pump system removed from the walking boot is shown in Figure 1. Through the reverse engineering process, it was discovered that the same air pump mechanism can be incorporated into the socket by making modifications to the mechanism. The vinyl on the bladders was removed, and the backing of the bladders and inner foam was cut down to the correct size. New vinyl was then glued onto the backing to create new bladders that fit inside of the socket
From the VELCRO® Brand Adhesives Guide, it was determined that the best VELCRO® for this socket is a strip with Adhesive 43 (Velcro Industries B.V., Manchester, NH). Adhesive 43 can be activated using iron-on heat. It can be bonded to most fabrics and plastics, has excellent water resistance, and is suitable for temperatures between -40°F to 160°F. The technical support department at VELCRO® USA Inc. was generous enough to donate VELCRO® strips with Adhesive 43 from their Sample Lab for use in this research.
Figure 1. Air pump system removed from a medical walking boot. The air pump system was modified to make the bladders small enough to fit inside of the socket. By incorporating the air pump system into the socket, the amputee will have the ability to adjust the tightness of the socket individually.
Finalized Three-Dimensional Models
The previous three-dimensional models for the two socket designs required alterations due to the changes in material selection. The final models reflect the material changes and include the addition of a cap at the end of the socket. The socket cap will allow the rest of the prosthetic device to attach to the socket. The cap will have a quick disconnect unit with a slide that allows the amputee to change the lower portion of the prosthetic based on his or her needs. The finalized three-dimensional models of the two socket designs are shown in Figures 2 and 3.
Detailed Drawings
To make the production process easier, detailed drawings of the three-dimensional socket models were created. The detailed drawings provide dimensions of the sockets and the scale of the drawing to the actual prosthetic. Figures 4 and 5 illustrate two of these detailed drawings.
RESULTS
Final Prosthetic Sockets
Using the aforementioned production plans and materials, the final prosthetic sockets were produced. The harness system and quick disconnect unit with a slide mechanism have not yet been incorporated into the sockets due to a lack of funds and time. However, both will be incorporated by the time the final products are delivered to the customers in Brazil. The final sockets are shown inFigures 6 and 7. The socket with the holes and air pump system includes a socket shell woven from wood dowels and natural sisal that is glued into the socket cap using epoxy. A modified air pump system and small pieces of piping glued into the weaving were also incorporated to increase airflow and modularity. For the open-frame socket, wooden stays were woven using wood dowels, natural sisal was glued into the slots of the socket cap using epoxy and a hot glue gun, and VELCRO® straps were attached to allow the amputee to adjust the fit.
Figure 2: Three-dimensional model of a socket with an air pump system and funnel-shaped holes. This socket design has an air pump system, similar to that used in medical walking boots, inside that allows the amputee to adjust the fit of the socket individually. The funnel-shaped holes around the entire wood socket shell allow maximum airflow to the residual limb, minimizing the risk of skin breakdown. A wood socket cap allows the socket to connect to the rest of the prosthetic. A COOLMAX® sock is slid over the residual limb before the socket to create a breathable socket interface.
Figure 3. Three-dimensional model of an open-frame socket with breathable material and VELCRO® straps. In this socket design, VELCRO® straps on the top and bottom of the structure allow the amputee to adjust the socket tightness individually. The VELCRO® straps are connected by four vertical wood stays, which creates an open-frame design that minimizes restriction and maximizes airflow to the residual limb. The socket cap and interface have the same design as those in Figure 2.
DISCUSSION AND CONCLUSIONS
After much research and discussion with professionals, it was decided that the most appropriate materials included Brazilian piacava wood, TENCEL® for the socket interface, VELCRO® straps with Adhesive 43, an air pump mechanism removed from a medical walking boot, and a wooden socket cap. For the purpose of this project, wood dowels were used in place of the Brazilian piacava wood, and a COOLMAX® sock was used for the socket interface.Detailed drawings, a bill of materials, and production plans were developed to assist with the manufacturing process. Finalized prosthetic sockets were then manufactured to satisfy the requirements. A harness system and quick disconnect unit will be incorporated before the prosthetic sockets are delivered to amputees in Brazil.
Figure 4. Detailed drawing of a socket with an air pump system and funnel-shaped holes. This detailed drawing illustrates how the socket components are assembled together in order to assist with the manufacturing process. Dimensions, including the diameter of the funnel-shaped holes, the diameter and thickness of the socket shell, and the thickness of the air pump system, can be extracted from this drawing.
Figure 5. Detailed drawing of an open-frame socket with breathable material and VELCRO® straps. This detailed drawing supplies information on dimensions and assembly of the socket components. Important measurements for the VELCRO® straps, wood stays, and socket shell are provided.
The lightweight design and breathability of the sockets is ideal for tropical climates where skin breakdown is highly probable. Their ease of use and modularity provide the amputees the ability to adjust the fit themselves, giving them more independence. Furthermore, the use of Brazilian piacava wood and TENCEL® from eucalyptus trees in future socket manufacturing will assist in creating jobs in underdeveloped areas of Brazil. In later designs, the prosthetic sockets can be modified to accommodate the climate conditions of other underdeveloped areas. This will allow countless amputees to receive prosthetic sockets during the first six months after amputation, increasing the chance of success with their prosthetics overall and providing them with greater independence.
Figure 6a. Completed prosthetic socket with air pump system and thin slices of piping to create airflow openings. (a) For the final product, wood dowels and natural sisal were used to weave a socket shell that was then glued into the wooden socket cap. It was quickly realized that drilling funnel-shaped holes into the socket was unrealistic, so thin pieces of piping were glued into the weaving to create airflow openings instead.
Figure 6b. Completed prosthetic socket with air pump system and thin slices of piping to create airflow openings. (b) A modified air pump system was glued into the socket shell to give the amputee the ability to adjust the socket fit independently.
Figure 7. Completed open-frame prosthetic socket with VELCRO® straps. For the final product, wood dowels and natural sisal were used to weave four wooden stays, which were then glued into the wooden socket cap. This created an open-frame design to allow maximum airflow to the residual limb. VELCRO® straps were attached to the top and bottom of the socket to improve the modularity of the socket.
Following discussions with Camila Nascimiento, an occupational therapist at the Centro de Reabilitação y Educação Adultos Humano (CREADH) clinic in Brazil, it was suggested that future sockets should use socket caps made of thermoplastic rather than wood (Camila Nascimiento, personal communication, June 5, 2014). Thermoplastic is a polymer that becomes flexible, or easily reshaped, when heated, and then solidifies when it is cooled, without compromising any of its properties or characteristics (Dictionary.com, 2015). Thermoplastic is easily reproducible and more accurate than attempting to recreate wood socket caps for each socket. The mold for the thermoplastic can be created in the United States, and the socket caps can then be produced in Brazil. Further discussions with occupational therapists, amputees, and caretakers in Brazil may lead to additional alterations and improvements to the socket designs.
ACKNOWLEDGEMENTS
Thank you to Dr. Jodi Prosise for her mentorship and assistance throughout the course of this research. Thank you to American Prosthetics and Orthotics in Davenport, IA, for providing examples of various upper limb prosthetic devices and assisting in the selection of materials and design concepts. Finally, thank you to all of the donors and fundraising that make St. Ambrose University’s Program for Assistive Technologies for the Underprivileged possible.
REFERENCES
Alley, R. D., Williams, T. W. III, Albuquerque, M. J., & Altobelli, D. E. (2011). Prosthetic sockets stabilized by alternating areas of tissue compression and release. Journal of Rehabilitation Research & Development, 48(6), 679-696. doi: 10.1682/ JRRD.2009.12.0197
Biddiss, E., Beaton, D., & Chau, T. (2007). Consumer designspriorities for upper limb prosthetics. Disability and Rehabilitation: Assistive Technology, 2(6), 346-357. doi: 10.1080/17483100701714733
Daly, W. (2000). Upper extremity socket design options. Physical Medicine and Rehabilitation Clinics of North America, 11(3), 627-638.
Dictionary.com, LLC. (2015). Thermoplastic. Retrieved Fromhttp://dictionary.reference.com/browse/thermoplastic.
Farago, J. A. & Skiffington, R. T. (2008). US Patent No. wood 2008057541 A2.
Jacobsen, S. C. & Knutti, D. F. (1999). US Patent No. 5,888,235. Salt Lake City, UT: Sarcos, Inc.
Kandhavadivu, P. (2013). Chapter 4: Influence of lyocell fiber blends on the comfort characteristics of hospital textiles. Retrieved from http://shodhganga.inflibnet.ac.in/bitstream/10603/9977/9/09_chapter%204.pdf
Männer, J., Schuster, K. C., Suchomel, F., Gürtler, A., & Firgo, H. (2004). Higher performance with natural intelligence. Lenzinger Berichte, 83, 99-110. Retrieved from http://faculty.mu.edu. sa/public/uploads/1346613242.2476LB-0832004099.pdf
Michaels, B. (2011). Regulating fluid transfer in wound-care applications. Medical Product Manufacturing News, 27(1). Retrieved from http://www.qmed.com/mpmn/article/regulatingfluid- transfer-wound-care-applications.
Norvell, J. (1996). US Patent No. 5480455 A. Newark, DE: W. L. Gore & Associates, Inc.
Østlie, K., Lesjø, I. M., Franklin, R. J., Garfelt, B., Skjeldal, O. H., & Magnus, P. (2012). Prosthesis rejection in acquired major upper-limb amputees: A population-based survey. Disability and Rehabilitation: Assistive Technology, 7(4), 294-303. doi: 10.3109/17483107.2011.635405
Ottobock© (2013). Above-elbow prosthesis with DynamicArm. Retrieved from http://www.ottobockus.com/prosthetics/ upper-limb-prosthetics/solution-overview/above-elbow-prosthesis- featuring-dynamicarm/.
Protective Packaging Corporation (2014). Moisture vapor transmission rate – MVTR. Retrieved from http://www.protectivepackaging. net/mvtr.
Sanders, J. E., Greve, J. M., Mitchell, S. B., & Zachariah, S. G. (1998). Material properties of commonly-used interface materials and their static coefficients of friction with skin and socks. Journal of Rehabilitation and Development, 35(2), 161-176.
Strait, E. (2006). Prosthetics in Developing Countries. (Unpublished doctoral dissertation).
Virginia Prosthetics (2014). Prosthetics fabrication. Retrieved from http://www.virginiaprosthetics.com/prosthetics_fabrication. html.
Visscher, M. O., Robinson, M., Fugit, B., Rosenberg, R. J., Hoath, S. B., & Wickett, R. R. (2011). Amputee skin condition: Occlusion, stratum corneum hydration and free amino acid levels. Archives of Dermatological Research, 303, 117-124. doi: 10.1007/s00403-010-1111-y.
Ziegler-Graham, K., MacKenzie, E. J., Ephraim, P. L., Travison, T. G., & Brookmeyer, R. (2008). Estimating the prevalence of limb loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation, 89(3), 422-429. doi: 10.1016/j.apmr.2007.11.005.