Author: Hasan Reem
Institution: Biology
Date: June 2002
When first confronted with the notion that viruses can cause cancer, many individuals react with suspicion. Traditionally, cancer is not thought of as an infectious disease; rather, it is presumed to be a result of a genetic predisposition to cancer, exposure to nuclear radiation or environmental toxins, or unhealthy eating and exercise habits. Most people are familiar with the widespread public health notices encouraging a healthy lifestyle as a method for substantially decreasing the likelihood that an individual will contract a serious illness such as cancer.
However, surprising as it may seem, viruses and other microbial agents also have been correlated directly with a significant proportion of cancer cases worldwide, according to prominent researchers in the field. The human papillomavirus (HPV), for example, is a virus that is implicated as a cause of cervical cancer. In contrast to health-promoting behavioral choices, we may not have control over exposure to the invisible cancer-causing viruses and microbial agents that have been linked to cancer.
Viruses in Cancer Research
Viruses have played an essential role in cancer biology research over the past several decades. At first, viruses were utilized as valuable laboratory research tools for understanding cell cycle controls and carcinogenesis, the origins and development of cancer. The use of viruses allowed researchers to unravel the genetics, mechanisms, and controls governing the processes of normal cell growth and differentiation. Viruses were also used to determine the role of aberrant cell growth or proliferation - processes characteristic of cancerous tissues.
Early research on retroviruses - RNA viruses that insert themselves into a host cell's DNA and then proliferate - allowed scientists to identify various regions of the genome most susceptible to carcinogenic mutations. Discovery of the "hot spots" of viral insertion led to an understanding of the genomic areas that could produce cancer-like replication rates of cells. Thus, in the research laboratory context, viruses were beneficial tools that expanded the scientific community's knowledge and understanding about basic mechanisms of normal and cancerous cells.
Viruses do not play a carcinogenic role only in experimental studies, however. The actual cancer-causing ability of some viruses has led to research in viral oncogenesis, or the origins and development of tumors. Cancer-causing viruses function much as non-carcinogenic viruses do, invading the living cells of the host and using its DNA-synthesizing proteins and mechanisms in order to produce more copies of itself. Then, the virus disrupts an integral cell-cycle control mechanism in order to render the infected cell and its progeny cancerous, or "hyper-proliferative." Uncontrolled cell replication or proliferation is the basis for oncogenesis.
Viruses and Cancer: The Case of HPV
There are variants of HPV known to play significant roles in the origins of cervical cancers, the second greatest cause of death in women due to cancer worldwide. Normally, benign variants of HPV exist within the human body, although the carcinogenic types are primarily spread through sexual interaction with another infected individual. The genomes of the harmful viruses contain different gene segments that code for several factors. Two such factors, known as E6 and E7, play roles in transforming the genes of the infected cell, effectively "immortalizing" it. Immortalization, or abnormal cell life cycle control involving continuous replication, is another way to describe the primary characteristic of cancer development. When E2, an inhibitory protein that usually keeps these factors under control, is rendered nonfunctional by the integrating virus, the E6 and E7 segments cause a transformation and proliferation of the infected cells and further spread the virus.
This results in several functional and physical changes in the infected cervical cells. As the layers of epithelium in the cervix mature and move toward the surface, the virus proliferates within the cells and is eventually expelled to the exterior as the cells reach the epithelial surface. After this, the virus can infect other cells. The effects of these viruses are manifested as lesions on the epithelial surface, detected by the common clinical technique known as a Pap smear.
In general, however, viruses have not been shown to be the sole carcinogenic agents in an individual; in most cases, many patients who are infected with viruses do not develop cancerous conditions. Indeed, the human body hosts hundreds of different types of viruses, and it is only in rare cases that this co-existent relationship is disturbed, with severe results including cancer. For example, the vast majority of people infected with HPV do not get cancer; in fact, less that 0.1% of infected individuals develop tumors. Often, viruses are able to generate their most serious effects in individuals who are immuno-compromised or physiologically unable to deter viral infection. According to Dr. Richard Schlegel, a scientist at the Georgetown University School of Medicine, the viruses mainly affect individuals who are unable to produce a cell-mediated response to the antigens presented by the virus-infected cells. This distinction likely plays a role in determining why the virus integrates into the host cell genome in some individuals and does not do so in others.
Determining the Role of Viruses
article_458_order_0
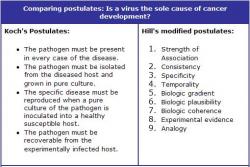
Because of these factors, it is difficult to state, in terms of disease risk, that a virus is the sole cause of the cancer development. Historically, to prove the causality between a substance and a disease or other condition, Koch's postulates must be satisfied. This task would involve isolating the virus, growing it in a culture, and then inducing the cancer in an animal and obtaining the same condition consistently under experimental laboratory conditions (see side bar). Because the challenge of growing certain viruses in a laboratory setting is great, this undertaking can be quite difficult. However, a more recent set of considerations formulated by Hill can also be employed to assess the epidemiological causality between the agent and the disease (see side bar). The criteria tested include strength of statistical association, consistency, dose-response relationship, coherence, specificity, and experimental evidence. Based on these considerations, several viruses can be considered to be the causal agents of various cancers. Epidemiological studies can be useful in validating associations with risk of disease in a human population. However, it is important to remember that while a virus may be implicated as the primary causal factor behind a certain type of cancer, its interaction and correlation with the presence or absence of other substances is also a significant factor in determining the risk of cancer development and its severity.
At present, more than 15 viruses have been shown to exist in a causal relationship with cancer. The most prominent of these include the Hepatitis B virus, Epstein-Barr virus, human papillomaviruses, human T-cell leukemia virus type I, and hepatitis C virus, which cause a variety of conditions, including liver, naso-pharyngeal, cervical, and skin cancers. The hepatitis viruses are known to cause 80% of liver cancer cases worldwide, and the papillomaviruses are responsible for the majority of cervical cancer cases. Overall, some researchers estimate that 15% of incident cases worldwide are in caused by viruses, and that of these cases, cancer appears to be a side effect, or risk associated with the original viral infection.
HPV Vaccines
Worldwide, there is a great deal of research currently in progress concerning the prevention and treatment of cervical cancer. It is estimated that about $6 billion is spent annually in the United States toward developing and producing an effective vaccine on a mass scale. This large amount of money is also the primary reason for the comparatively low cervical cancer death rate in the United States; the combined effect of routine screening and early treatment promotes greater survival.
In other areas of the world, the mortality associated with HPV infection is much more serious, making it the primary cause of the 400,000 annual cervical cancer deaths worldwide. These nations lack the resources to promote and implement a major screening program similar to the program that exists in the United States.
Presently, a first-generation vaccine exists for HPV; however, at approximately $100 per dose, it is inaccessible to residents of most developing nations. To further complicate the problem, these countries have the greatest need for the vaccines, as their prevention guidelines are less ordered and systematic than the programs existing in the United States and other developed countries.
Dr. Schlegel's laboratory at Georgetown University Medical Center is involved in the development of a cheap and effective vaccine. This vaccine is currently undergoing clinical trials to determine its usefulness in humans. In previous trials on dogs, it has already been shown as a protective factor against infection with the virus, and a similar conclusion is expected in the human population.
Summary
Whereas the idea of cancer-causing viruses may sound dubious at first, several viruses do indeed play a significant role in the prevalence of cancer worldwide, including HPV, Epstein-Barr virus, and Hepatitis B virus. Many of these viruses are infectious, often spread through sexual contact with another individual. However, they have their greatest effects in immuno-compromised individuals, those who are unable to initiate their cell-mediated immune responses, or are otherwise unable to effectively fight off the infection even after identification of cancerous cells. In developed nations, screening and other prevention techniques have been used with great success to detect infections early, specifically with regard to HPV. Cheap and effective vaccines are currently in development for easy distribution worldwide, and this appears to be a critical development for successful control of the spread of viruses such as HPV and their associated cancers.
Suggested Reading
Butel JS. "Viral carcinogenesis: revelation of molecular mechanisms and etiology of human disease." Carcinogenesis: 21 (2000): 405-426.
Epidemiologic Tenets of Causality. Course Website, PH1820 - Statistical Analysis Fall 2001, University of Texas School of Public Health. 2 May 2002. http://www.sph.uth.tmc.edu:8053/Biometry/LMoye/StatAnalysis%202001/PH1820%202001/epid1.htm
Schecter WP. "Human immunodeficiency virus and malignancy: thoughts on viral oncogenesis". Archives of Surgery. 136 (2001): 1419-25.